 I am going to lead with both feet here…I am a survivor of suicide. By that I mean, someone very close to me, in fact several people I had the pleasure of knowing for only too short of a time, have committed suicide. On the surface, they seemed like normal, everyday people who had no ‘good’ reason to kill themselves and appeared to be very strong, capable people. You would never in a million years, have thought that they would commit suicide. But they did. I write this article during September, which is Suicide Prevention Month, in their honor and hope that someone reading this article may be able to step in and help prevent someone from committing suicide and maybe, just maybe, give someone hope in the face of the yawning blackness.
I am going to lead with both feet here…I am a survivor of suicide. By that I mean, someone very close to me, in fact several people I had the pleasure of knowing for only too short of a time, have committed suicide. On the surface, they seemed like normal, everyday people who had no ‘good’ reason to kill themselves and appeared to be very strong, capable people. You would never in a million years, have thought that they would commit suicide. But they did. I write this article during September, which is Suicide Prevention Month, in their honor and hope that someone reading this article may be able to step in and help prevent someone from committing suicide and maybe, just maybe, give someone hope in the face of the yawning blackness.
For immediate assistance for you or someone else there is a national hotline number:
1-800-273 TALK (8255)
Vet2Vet Talk Line 1-855-838-7481
If you don’t wish to talk to someone unknown, then please call a friend or family member to talk.
Suicide is not an act of cowardice nor an act of selfishness. It is not directed at any individual or person in the life of the person who is contemplating or has committed suicide. It is not personal. It is an act of desperation borne out of hopelessness that someone feels is insurmountable. The best way I have seen and heard it put is that someone contemplating suicide is in a deep, tarry pit of blackness with no light.
It is a fact that 90% of people who, at the time they commit or attempt to commit suicide have a diagnosable and TREATABLE mental health issues.
Risk factors include:
Biggest risk factor is clinical depression
Undiagnosed or untreated mental health issues
Family history of suicide
Knowing someone (close) who has committed suicide
Family history of child neglect/abuse
History of abuse (domestic, sexual assaults)
History of brain injury
History of traumatic experiences
Previous suicide attempt(s)
History of alcohol and substance abuse
Feelings of hopelessness
Impulsive or aggressive tendencies
Isolation, a feeling of being cut off from other people
Barriers to accessing mental health treatment
Loss (relational, social, work, or financial)
Physical illness
Easy access to lethal methods
Unwillingness to seek help because of the stigma attached to mental health and substance abuse disorders or to suicidal thoughts
Suicidal ideation
Risk factors do not indicate that someone will commit suicide, just that their chances of committing suicide increase.
Prevention and intervention become key.
There are twice as many suicides in the US than homicides. For everyone person who completes suicide, approximately another 12 attempt suicide. WHO (World Health Organization) estimates that approximately 1 million people around the world commit suicide yearly. Many who attempt suicide never receive any help.
Know the warning signs. The best way to prevent suicide is to recognize the warning signs and how to respond if you spot them. If you believe that a friend or family member is suicidal, you can play a role in suicide prevention by pointing out the alternatives, showing that you care and are there to listen to them without judgment, and getting a doctor or psychologist involved, if they are willing.
In my own time of answering a hotline the biggest help I was able to give someone was just listening to them. Not providing answers unless directly asked nor arguing with them about how they felt. Learning how to listen without taking charge or downplaying someone’s feelings is essential in helping.
The below has been taken directly from and more information can be found at : Help Guide
Major warning signs for suicide include talking about killing or harming oneself, talking or writing a lot about death or dying, and seeking out things that could be used in a suicide attempt, such as weapons and drugs. These signals are even more dangerous if the person has a mood disorder such as depression or bipolar disorder, suffers from alcohol dependence, has previously attempted suicide, or has a family history of suicide.
Take any suicidal talk or behavior seriously. It’s not just a warning sign that the person is thinking about suicide—it’s a cry for help.
A more subtle but equally dangerous warning sign of suicide is hopelessness. Studies have found that hopelessness is a strong predictor of suicide. People who feel hopeless may talk about “unbearable” feelings, predict a bleak future, and state that they have nothing to look forward to.
Other warning signs that point to a suicidal mind frame include dramatic mood swings or sudden personality changes, such as going from outgoing to withdrawn or well-behaved to rebellious. A suicidal person may also lose interest in day-to-day activities, neglect his or her appearance, and show big changes in eating or sleeping habits.
Talking about suicide
Any talk about suicide, dying, or self-harm, such as “I wish I hadn’t been born,” “If I see you again…” and “I’d be better off dead.”
Seeking out lethal means Seeking access to guns, pills, knives, or other objects that could be used in a suicide attempt.
Preoccupation with death Unusual focus on death, dying, or violence. Writing poems or stories about death.
No hope for the future Feelings of helplessness, hopelessness, and being trapped (“There’s no way out”). Belief that things will never get better or change.
Self-loathing, self-hatred Feelings of worthlessness, guilt, shame, and self-hatred. Feeling like a burden (“Everyone would be better off without me”).
Getting affairs in order Making out a will. Giving away prized possessions. Making arrangements for family members.
Saying goodbye Unusual or unexpected visits or calls to family and friends. Saying goodbye to people as if they won’t be seen again.
Withdrawing from others Withdrawing from friends and family. Increasing social isolation. Desire to be left alone.
Self-destructive behavior Increased alcohol or drug use, reckless driving, unsafe sex. Taking unnecessary risks as if they have a “death wish.”
Sudden sense of calm A sudden sense of calm and happiness after being extremely depressed can mean that the person has made a decision to commit suicide.
Suicide prevention tip #1: Speak up if you’re worried
If you spot the warning signs of suicide in someone you care about, you may wonder if it’s a good idea to say anything. What if you’re wrong? What if the person gets angry? In such situations, it’s natural to feel uncomfortable or afraid. But anyone who talks about suicide or shows other warning signs needs immediate help—the sooner the better.
Talking to a person about suicide
Talking to a friend or family member about their suicidal thoughts and feelings can be extremely difficult for anyone. But if you’re unsure whether someone is suicidal, the best way to find out is to ask. You can’t make a person suicidal by showing that you care. In fact, giving a suicidal person the opportunity to express his or her feelings can provide relief from loneliness and pent-up negative feelings, and may prevent a suicide attempt.
Ways to start a conversation about suicide:
• I have been feeling concerned about you lately.
• Recently, I have noticed some differences in you and wondered how you are doing.
• I wanted to check in with you because you haven’t seemed yourself lately.
Questions you can ask:
• When did you begin feeling like this?
• Did something happen that made you start feeling this way?
• How can I best support you right now?
• Have you thought about getting help?
What you can say that helps:
• You are not alone in this. I’m here for you.
• You may not believe it now, but the way you’re feeling will change.
• I may not be able to understand exactly how you feel, but I care about you and want to help.
• When you want to give up, tell yourself you will hold off for just one more day, hour, minute—whatever you can manage.
When talking to a suicidal person
Do:
• Be yourself. Let the person know you care, that he/she is not alone. The right words are often unimportant. If you are concerned, your voice and manner will show it.
• Listen. Let the suicidal person unload despair, ventilate anger. No matter how negative the conversation seems, the fact that it exists is a positive sign.
• Be sympathetic, non-judgmental, patient, calm, accepting. Your friend or family member is doing the right thing by talking about his/her feelings.
• Offer hope. Reassure the person that help is available and that the suicidal feelings are temporary. Let the person know that his or her life is important to you.
• If the person says things like, “I’m so depressed, I can’t go on,” ask the question: “Are you having thoughts of suicide?” You are not putting ideas in their head, you are showing that you are concerned, that you take them seriously, and that it’s OK for them to share their pain with you.
But don’t:
• Argue with the suicidal person. Avoid saying things like: “You have so much to live for,” “Your suicide will hurt your family,” or “Look on the bright side.”
• Act shocked, lecture on the value of life, or say that suicide is wrong.
• Promise confidentiality. Refuse to be sworn to secrecy. A life is at stake and you may need to speak to a mental health professional in order to keep the suicidal person safe. If you promise to keep your discussions secret, you may have to break your word.
• Do NOT Offer ways to fix their problems, or give advice, or make them feel like they have to justify their suicidal feelings. It is not about how bad the problem is, but how badly it’s hurting your friend or loved one.
• Blame yourself. You can’t “fix” someone’s depression. Your loved one’s happiness, or lack thereof, is not your responsibility.
Adapted from: Metanoia.org
Suicide prevention tip #2: Respond quickly in a crisis
If a friend or family member tells you that he or she is thinking about death or suicide, it’s important to evaluate the immediate danger the person is in. Those at the highest risk for committing suicide in the near future have a specific suicide PLAN, the MEANS to carry out the plan, a TIME SET for doing it, and an INTENTION to do it.
The following questions can help you assess the immediate risk for suicide:
• Do you have a suicide plan? (PLAN)
• Do you have what you need to carry out your plan (pills, gun, etc.)? (MEANS)
• Do you know when you would do it? (TIME SET)
• Do you intend to commit suicide? (INTENTION)
If a suicide attempt seems imminent, call 1-800-273-TALK(8255), dial 911, or take the person to an emergency room. Remove guns, drugs, knives, and other potentially lethal objects from the vicinity but do not, under any circumstances, leave a suicidal person alone.
Level of Suicide Risk
Low — Some suicidal thoughts. No suicide plan. Says he or she won’t commit suicide.
Moderate — Suicidal thoughts. Vague plan that isn’t very lethal. Says he or she won’t commit suicide.
High — Suicidal thoughts. Specific plan that is highly lethal. Says he or she won’t commit suicide.
Severe — Suicidal thoughts. Specific plan that is highly lethal. Says he or she will commit suicide.
Suicide prevention tip #3: Offer help and support
If a friend or family member is suicidal, the best way to help is by offering an empathetic, listening ear. Let your loved one know that he or she is not alone and that you care. Don’t take responsibility, however, for making your loved one well. You can offer support, but you can’t get better for a suicidal person. He or she has to make a personal commitment to recovery.
It takes a lot of courage to help someone who is suicidal. Witnessing a loved one dealing with thoughts about ending his or her own life can stir up many difficult emotions. As you’re helping a suicidal person, don’t forget to take care of yourself. Find someone that you trust—a friend, family member, clergyman, or counselor—to talk to about your feelings and get support of your own.
Helping a suicidal person:
• Get professional help. Do everything in your power to get a suicidal person the help he or she needs. Call a crisis line for advice and referrals. Encourage the person to see a mental health professional, help locate a treatment facility, or take them to a doctor’s appointment.
• Follow-up on treatment. If the doctor prescribes medication, make sure your friend or loved one takes it as directed. Be aware of possible side effects and be sure to notify the physician if the person seems to be getting worse. It often takes time and persistence to find the medication or therapy that’s right for a particular person.
• Be proactive. Those contemplating suicide often don’t believe they can be helped, so you may have to be more proactive at offering assistance. Saying, “Call me if you need anything” is too vague. Don’t wait for the person to call you or even to return your calls. Drop by, call again, invite the person out.
• Encourage positive lifestyle changes, such as a healthy diet, plenty of sleep, and getting out in the sun or into nature for at least 30 minutes each day. Exercise is also extremely important as it releases endorphins, relieves stress, and promotes emotional well-being.
• Make a safety plan. Help the person develop a set of steps he or she promises to follow during a suicidal crisis. It should identify any triggers that may lead to a suicidal crisis, such as an anniversary of a loss, alcohol, or stress from relationships. Also include contact numbers for the person’s doctor or therapist, as well as friends and family members who will help in an emergency.
• Remove potential means of suicide, such as pills, knives, razors, or firearms. If the person is likely to take an overdose, keep medications locked away or give out only as the person needs them.
• Continue your support over the long haul. Even after the immediate suicidal crisis has passed, stay in touch with the person, periodically checking in or dropping by. Your support is vital to ensure your friend or loved one remains on the recovery track.
I will also add this: do NOT be afraid to advocate for them with the mental health system. In many states it can take a lot to make sure someone with a mental health issue gets the care that they need. But you can do it and so can they!
As a final note: PTSD is becoming increasing a high risk factor in terms of suicide. The very nature of PTSD and the way it is conceived makes it difficult for those suffering with PTSD to reach out and get the help they need. And many people suffering from PTSD are our returning Veterans. It is believed that approximately every 65 minutes one of our returning Veterans commits suicide. If you are a veteran, a family member or a friend of Veteran, please let them know you are there for them and will help them.
Phone numbers and resources:
Suicide prevention hotline: 1-800-273-TALK(8255)
When you dial 1-800-273-TALK (8255), you are calling the crisis center in the Lifeline network closest to your location. After you call, you will hear a message saying you have reached the National Suicide Prevention Lifeline. You will hear hold music while your call is being routed. You will be helped by a skilled, trained crisis worker who will listen to your problems and will tell you about mental health services in your area. Your call is confidential and free.
In an EMERGENCY call 911
Veterans Crisis Line
this is for veterans, guardsmen, friends and family members of those who have served our country
1-800-273-8255 and Press 1
Or send a text message to 838255
Vet2Vet Talk Line 1-855-838-7481
The Vet2Vet Talk Line (1-855-838-7481) provides 24/7 confidential peer support, information and referrals for all of America’s Veterans and their families. Every call is answered by a Veteran who understands the rewards and challenges of military service and is trained to provide compassionate and caring peer support along with access to a wide array of services across the nation.
Need help finding a qualified therapist in your area?
The link above will take you directly to a ‘find a therapist’ page. The therapists listed here all specialize in anxiety/depressive disorders.
No one willingly wants to die…it is not human nature…human nature is about survival and sometimes we need help. Don’t be alone or afraid anymore.
God Bless and Keep You
survivingshtfmom
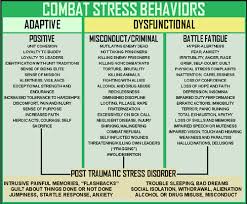
 Kind of tongue in cheek title, but with all do seriousness, I made it that way in an effort to make you think. PTSD symptoms do not happen in a vacuum. They might fade, disappear for a time but they never truly go ‘away’ forever. Think of it this way, the brain is like computer with a CD Rom that is always recording what is going on. When a traumatic event happens that too gets burned onto the CD. A trigger is like a command prompt or a file connected to the original event which then gets replayed. Or more simply put, a trigger is like pushing the on button unintentionally.
Kind of tongue in cheek title, but with all do seriousness, I made it that way in an effort to make you think. PTSD symptoms do not happen in a vacuum. They might fade, disappear for a time but they never truly go ‘away’ forever. Think of it this way, the brain is like computer with a CD Rom that is always recording what is going on. When a traumatic event happens that too gets burned onto the CD. A trigger is like a command prompt or a file connected to the original event which then gets replayed. Or more simply put, a trigger is like pushing the on button unintentionally.




Stress and Infectious Diseases: STOP THE STRESS!!!
Our immune system is what keeps us from having to live a sterile environment and it’s in our best interest to keep our immune system strong so that when some invaders comes a knockin’ we have a fighting chance to live. I would hazard to guess that most people don’t even THINK about their immune system and what would happen if it went bye-bye or was seriously compromised. Day in and day out we go about our lives full of stress and surrounded by germs. So, in this day and age when we typically don’t eat right, sit around a lot and stress out about everything and ding our immune systems with literally hundreds of different chemicals everyday what can we do to support our immune system? Fight STRESS!!!
Stress…stress can kill you and that isn’t a joke…according to Paige Bierma, M.A
“Some kinds of stress — very short-term, that last only a matter of minutes — actually redistribute cells in the bloodstream in a way that could be helpful,” says Suzanne Segerstrom, an associate professor of psychology at the University of Kentucky who has conducted studies on stress and the immune system. “But once stress starts to last a matter of days, there are changes in the immune system that aren’t so helpful. And the longer that stress lasts, the more potentially harmful those changes are.”
The fight-or-flight response (short-term stress) goes something like this: When a villager in Africa sees a lion charging at him, for example, the brain sends a signal to the adrenal gland to create hormones called cortisol and adrenaline, which have many different effects on the body, from increasing heart rate and breathing to dilating blood vessels so that blood can flow quickly to the muscles in the legs. Besides helping him run away, this type of acute stress also boosts the immune response for three to five days (presumably to help him heal after the lion takes a swipe at him).
When humans experience stress, our bodies react the same way that animals’ bodies do. Once the lion is gone, a zebra or gazelle’s stress level will return to normal, but humans have more trouble getting back to our routines after a stressful event, whether it’s a car accident or a divorce. We’ll think about it, dream about it, and worry about it for a long time, and that sets us up for long-term problems, says Robert M. Sapolsky, a Stanford University stress expert and author of Why Zebras Don’t Get Ulcers.
Over time, continually activating the stress response may interfere with the immune system. How this affects your disease risk, Sapolsky suggests, depends partly on your risk factors and your lifestyle, including your degree of social support.
Infectious disease and stress:
A number of vaccine studies have also found that the immune system of highly stressed individuals have sluggish responses to challenges. In one study, published in the journal Psychosomatic Medicine, a pneumonia vaccine was administered to 52 older adults, including 11 people caring for spouses with dementia. After just six months, the levels of antibodies produced against pneumonia in the caregivers had dropped off, while the non-caregivers’ levels remained stable. A similar study in which 32 caregivers were given the flu shot also found that caregivers received less protection from the vaccine than did a control group of non-caregivers.
If you’re stressed out, you’re more likely to get sick — at least it seems that way. A study in the New England Journal of Medicine actually found that higher psychological stress levels resulted in a higher likelihood of catching the common cold. The researchers accounted for many variables — including the season; alcohol use; quality of diet, exercise, and sleep; and levels of antibodies before exposure to the virus — and concluded that higher stress was to blame for lowered immunity and higher infection rates.
In the meantime, there is enough evidence to convince us that we should find healthy ways to keep our stress levels down, which is advice we got from our grandmothers: Eat right, exercise, and get enough sleep.
“Stress is inevitable,” Spiegel says. “The trick is to learn to manage it, to find some aspect of our stress and do something about it. Don’t think in terms of ‘all or nothing’ but in terms of ‘more or less.’ ”
An immune system that is continually ‘working, working, working’ never gets a chance to recover so when challenged by an invader it cannot mount an adequate defense.
Learn to manage your stress!
Stressful events are a fact of life and they can be even little ones like too much noise or activity going on around you. You can learn to identify what stresses you and how to take care of yourself physically and emotionally in the face of stressful situations. Learn to UNWIND in a healthy way.
Stress management strategies include:
Eating a healthy diet and getting regular exercise and plenty of sleep
Practicing relaxation techniques or learning to meditate
Fostering healthy friendships
Having a sense of humor
Seeking professional counseling when needed
Learn to say no! Set yourself realistic expectations and learn how to say “no” when your workload or social and family commitments get too much.
Learn to switch off. Leaving the office for the day? Then it’s time to switch off your work brain as well as your mobile phone. Unless you need to be on call for work, there’s rarely anything that can’t be solved the next day with renewed perspective.
Breathe! When we’re stressed, we tend to shallow breathe. Try to take deeper breaths into your diaphragm.
But hey! There is good news on the stress/immune system relation using herbs called adaptogens and these can be included into your healthy diet as herbal supplements. According to Frank M. Painter, D.C.:
The body expends a great amount of energy keeping itself in a heightened state of readiness. When weakened by prolonged stress–be it caused by lack of sleep, poor diet, chemical toxins in the environment or mental assaults–the body’s ability to maintain homeostasis can be compromised, and illness can result. Adaptogenic herbs have traditionally helped prevent the imbalances that can result from stress and have therefore prevented or minimized disease. At the core of an adaptogen’s scope of actions is the ability to help the body cope more effectively with stress. Specifically, adaptogens recharge the adrenal glands, which are the body’s nominal mechanism for responding to stress and emotional changes. The adrenals, which cover the upper surface of each kidney, synthesize and store dopamine, norepinephrine and epinephrine. These compounds are responsible for the changes that occur during the fight-or-flight reaction.
Well known adaptogenic herbs are:
Ginseng
Suma
Ashwaganda
Astragalus
Schisandra
Jiaogulan
And while mushrooms are not technically herbs Reishi, shiitake, maitake mushrooms have been shown to have adaptogen properties also.
Homeopathy can also play a role in reducing stress levels when needed and be apart of an overall stress reduction program:
According to Claire Zarb LCPH, it’s advisable to start with a 30c potency and take every hour or so when the feelings of stress are at their peak.
Argentum Nitricum
Ideal for treating anxiety, caused by the anticipation of a big event, such as an exam, party or public speaking event. Dizziness and diarrhea may also be experienced, especially in the morning. People who need this remedy are often enthusiastic and suggestible, with a tendency towards being quite impulsive. They often crave sweets which usually make their symptoms worse.
Gelsemium
When a dull, heavy, but restless, weariness dominates you, think of Gelsemium. A dose before an exam or interview can keep your mind from drawing a blank. Heavy fatigue with muscular weakness means it’s great for flu, restless colds, diarrhea and dull, pressing headaches. This can be a very steadying remedy, especially to quiet, often low-spirited people who dread public speaking.
Nux Vomica
This remedy’s reputation is based on its ability to treat modern day complaints of indigestion, intoxication, and stress. Nux Vomica acts to neutralize both the effect of stress on the mind, and excess intake of food, alcohol and drugs on the digestive system. Nux Vomica offers comfort when travel, hangovers, busy schedules, overwork, or late night meals cause digestive and mental distress. Ideal if you’re a ‘workaholic’ who is easily irritable and tired.
Lycopodium
Ideal for nerves and indecision and especially good if you worry a lot and battle with self-confidence (too much and too little!). Digestively, it applies to acidity, gas, bloating, colic and constipation. There may be a fear of change, irritability, obstinacy, stage fright and exam nerves.
And don’t forget the Food!
According to Michael Ozner, MD, the top 10 stress fighting foods are:
1. Spinach contains magnesium, which helps improve your body’s response to stress and may prevent migraine headaches.
2. Asparagus is a good source of folic acid, which produces serotonin and helps stabilize mood.
3. Beef helps stabilize mood by supplying zinc, iron, and B vitamins.
4. Dairy products such as milk and cottage cheese provide protein and calcium.
5. Nuts and seeds are good stress-fighting snacks. In addition to containing vitamin B12, magnesium, and zinc, almonds also provide vitamin E, which, like vitamin C, fights stress-related free radicals that cause heart disease. Walnuts and pistachios are known to lower blood pressure. Sunflower seeds include folate, which helps produce dopamine, a pleasure-inducing brain chemical.
6. Fruits such as oranges and blueberries contain vitamin C, which fights cancer-causing free radicals. Blueberries also counteract the effect of hormones such as cortisol, and bananas provide potassium, which lowers blood pressure.
7. Fish containing omega-3 fatty acids, such as salmon, can boost serotonin levels and limit the production of anxiety hormones such as adrenaline and cortisol.
8. Avocados are a good source of monounsaturated fat and potassium, which lower blood pressure.
9. Milk, including skim milk, is high in antioxidants and vitamins B2 and B12 and also provides protein and calcium, which can reduce muscle spasms and tension and soothe PMS.
10. Crispy rice cereal or corn flakes aren’t necessarily low in sugar; however, they offer B vitamins and folic acid, which reduce stress. Have a bowl of whole-grain cereal with milk for a stress-fighting breakfast.
Four foods to avoid:
1. Caffeine, found in coffee, tea, soda, and chocolate, can cause anxiety and raise stress hormone levels.
2. Sugar causes spikes in blood glucose levels and increases insulin. This affects your adrenal glands, which regulate stress hormones and help the thyroid regulate body weight.
3. Trans fatty acids such as hydrogenated vegetable oil are found in many baked goods and can hinder the immune system and increase the risk of heart disease.
4. Alcohol puts more sugar in the body, and excessive consumption can damage the adrenal glands.
While stress is just one factor in keeping the immune system healthy you can see that there are ways of helping the body to defend itself against stress and boost our body’s resiliency against stress. So get moving, eat ‘right’ and get your SLEEP and don’t forget to add homeopathy and herbs into your life to LIVE! Your immune system will love you!
Stay safe, be prepared!
survivingshtfmom